Articles
Hydrogen sulfide could help people with diabetes recover from heart and blood vessel complications.
Rotten egg gas could help protect diabetics from heart complications
A gas that was formerly known for its noxious qualities could help people with diabetes recover from heart and blood vessel complications, concludes research led by the University of Exeter Medical School.
The research could help pave the way to new treatments for some of the most common complications association with diabetes. Heart problems are a common cause of disability and death in people with diabetes, and are expected to rise still further with increasing rates of obesity. Currently, 79% of the £14 billion spent on treating diabetes in the NHS is spent on treating complications.
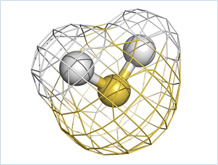
Laboratory research published in Pharmacological Research and funded by the European Union and Medical Research Council has yielded promising results from new drugs which selectively target minute quantities of the foul smelling gas hydrogen sulfide inside blood vessel cells. Research indicates the drugs AP39 and AP123 could help prevent sugar (glucose) from damaging endothelial cells, which line blood vessels and form an interface that regulates the exchanges of materials such as oxygen and food metabolites between blood and surrounding tissue.
People with diabetes have an excess of glucose in their blood (hyperglycaemia). This leads to the mitochondria, the “power house” of the cell which normally regulates energy production and use inside cells very tightly, becoming inefficient and leaky. They then produce highly toxic metabolites of oxygen (free radicals). The resulting toxicity to the mitochondria in the endothelial cells damages blood vessels in the circulation and the heart. This can deprive organs of the blood they need to function, potentially resulting in kidney disease or retinopathy, which cause blindness. Around 1,280 cases of blindness causes by diabetes each year in England alone, with a further 4,200 people identified as at risk of vision loss from this cause. Damaged blood vessels can also contribute to kidney disease, which can affect up to one in three people with diabetes.
Now, research using endothelial cells isolated from the small blood vessels in the brains of mice has revealed that carefully targeting minute quantities of hydrogen sulfide to the mitochondria inside cells using AP39 or AP123 restored the efficiency of the mitochondria and prevented hyperglycaemia-induced build up of free radicals. The team found that the effects of the drugs were long-lasting, suggesting that they could help to treat heart problems and blood vessel complications that occur in the heart, kidney and eyes of people with diabetes.
Professor Matthew Whiteman, of the University of Exeter Medical School, who led the study, said: “We’re producing a growing body of evidence that hydrogen sulfide can have a range of health benefits, when carefully administered in minute doses in a highly targeted way in the body. Mitochondria can even make their own hydrogen sulfide and use it as a ‘fuel’ to keep metabolism efficient. When this ‘fuel’ is lost, mitochondria, cells, blood vessels and tissues are damaged. We previously showed that replacing the lost hydrogen sulfide with AP39 reversed this damage in cardiac arrest, hypertension and kidney failure damage and this current study adds AP123 to our portfolio of promising new drugs for diabetes.
“Some people find it amusing that a substance with such a bad reputation can produce these benefits, but nearly every cell in our body makes and responds to tiny amounts of hydrogen sulfide and we have at least three distinct pathways for making this gas in very small quantities so it is very important. We must now continue working hard towards taking our findings forward in humans”.
The paper, ‘The novel mitochondria-targeted hydrogen sulfide (H2S) donors AP123 and AP39 protect against hyperglycemic injury in microvascular endothelial in vitro’ is published in Pharmacological Research. Authors are Domokos Gerö, Roberta Torregrossa, Alexis Perry, Alicia Waters, Sophie Le Trionnaire, Jacqueline L. Whatmore, Mark Wood, Matthew Whiteman.
Date: 1 September 2016
