Articles
The new grant helps research into haemochromatosis
A £300,000 boost for research into an iron overload genetic condition
New funding will help researchers unlock questions about the common genetic iron overload condition, haemochromatosis. They will study the longer-term impact of the faulty gene on the body and brain, and find out why some people with the faulty gene are much more severely affected than others.
It was thought that less than one percent of those with the faulty genes developed the condition. However, earlier this year, research by the University of Exeter Medical School showed that by age 63, one in five men (20%) with the faulty gene were diagnosed with a related disease, plus one in ten of women (10%). The faulty genes increases risks of severe fatigue, joint and muscle pains, arthritis, diabetes, and liver disease. Over 250,000 people in the UK have the two copies of the faulty genes needed to cause haemochromatosis, making it the most common genetic condition in the UK.
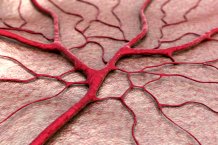
Now the Exeter team has received £291,000 from the government’s UK Medical Research Council (MRC) for research into why the disease is more severe in some, and on the longer-term effects of the faulty genes on diseases such as dementia and diabetes. The genes (called HFE C282Y) cause excessive iron to be absorbed from the diet. The excess iron can be treated in the same way as donating blood, as blood is rich in iron. The disease is often difficult for doctors to spot as it has few distinguishing features, but the high iron levels are easy to test for and the treatment is effective and safe if started early. However, many patients are currently only diagnosed after irreversible condition has developed.
Lead applicant, Professor David Melzer of The University of Exeter said: “A key question for us is what makes the condition severe in only a minority of the people with the faulty genes. This funding will help us identify which patients are at most risk, so that they can be diagnosed and treated earlier. The funding will also help us learn more about the longer-term effects of the faulty genes, including on the brain.”
Chief Exec. of Haemochromatosis UK, David Head said: “We have suspected for many years that the impact of genetic iron overload is much greater that has been assumed by many healthcare professionals, so we are absolutely delighted with Professor Melzer’s interest in the broad impact of iron and the C282Y mutation. We believe that the prevalence and significant impact of iron overload on people’s lives - especially for older people - mean that haemochromatosis should be much higher on the healthcare agenda in the UK than it is. It is well-founded research like this that will provide the hard evidence needed to stimulate the investment that is needed in early diagnosis and thus prevention of many chronic follow-on effects."
He added: “It’s particularly interesting to see research into the effects of iron on the brain, and links to other conditions such as dementias and muscle wastage. It’s also fascinating that compared to previous studies, such a large amount of data is being analysed; whatever the outcomes of this work, we can be confident that it will be very robust.”
The high iron levels caused by the haemochromatosis faulty genes have been linked to many diseases, including liver cirrhosis and cancers, severe arthritis, and diabetes. The team will search for other genes and also health risks which may increase the chances of developing serious disease in people with the main faulty genes. Approximately one in eight people in the UK study are carriers of the gene, meaning they had one faulty gene, but related disease is rare in carriers. If both parents are carriers then two faulty genes can be passed on to their children.
Symptoms of haemochromatosis can include feeling tired all the time, muscle weakness and joint pains, meaning it is often misdiagnosed as the signs of ageing. Haemochromatosis accounts for over one percent of all hip replacements, arthritis, diabetes and liver disease in 60 to 70 year olds.
Haemochromatosis is treatable with regular removal of blood, known as a venesection. This is usually carried out once every few weeks. When the iron levels are lowered, this reduces to around four times per year. This is known as maintenance therapy. Blood can be donated once the patient's iron levels reach maintenance.
The grant is funding a researcher, Dr Janice Atkins, to study data from the UK Biobank, a database containing genetic data of 500,000 people across England, Scotland and Wales. This database is used to improve the prevention, diagnosis and treatment of a wide range of serious and life-threatening illnesses.
The NHS advises that it is important to talk to your GP if you have a parent or sibling with haemochromatosis, even if you don't have symptoms yourself – tests can easily be done to check if you're at risk of developing problems. People are also advised to talk to their GPs about haemochromatosis if they have the following persistent or worrying symptoms – particularly if you have a northern European family background. Typical symptoms include feeling very tired all the time (fatigue); weight loss; weakness and joint pain. Also, some men with haemochromatosis develop an inability to get or maintain an erection (erectile dysfunction), and some women have irregular periods or absent periods. These symptoms often come on between ages 30 and 60, but can develop at older ages.
Date: 28 May 2019
